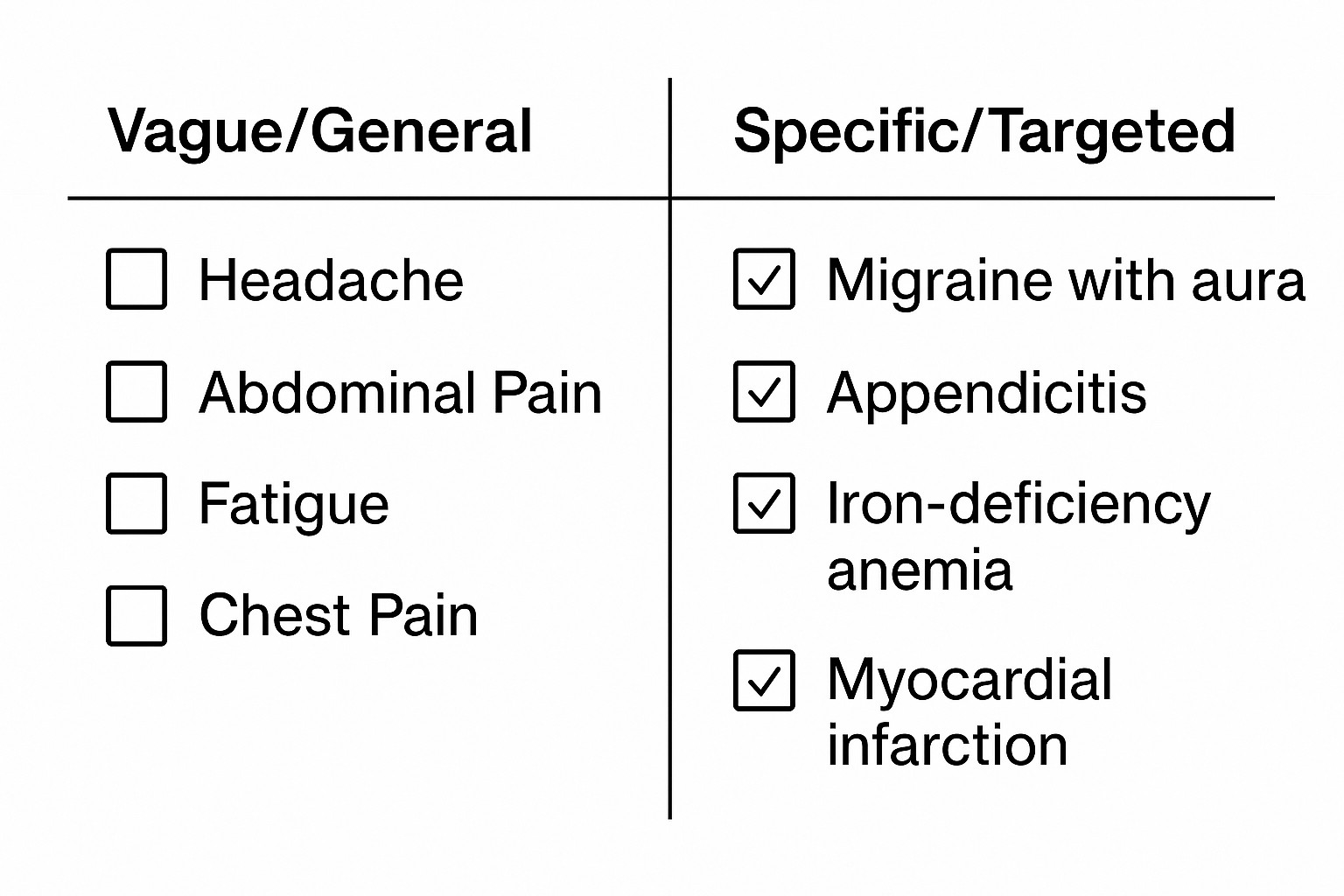
In today’s healthcare environment, precision matters. Vague diagnoses don’t just impact patient care—they can delay reimbursements, increase audit risk, and undermine risk adjustment capture, which is necessary for both clinical and financial accuracy.
Leading organizations, including AMA, CMS, CDC, AAPC, AHIMA, and AAFP, emphasize that coding to the highest level of specificity is not optional—it’s essential. For healthcare providers, this ensures that care, documentation, and reimbursement all align with the true complexity of patients’ conditions.
Why Specificity Matters
Accurate, specific diagnoses are the backbone of quality care and correct reimbursement.
- Patient Care: The more detailed the documentation, the better clinicians can manage chronic conditions, tailor treatment plans, and anticipate complications.
- Compliance and Audits: CMS and AHIMA note that unspecified or vague codes can trigger audits and create compliance challenges.
- Risk Adjustment Capture: Risk adjustment models, like CMS-HCC, rely on complete and specific documentation to reflect a patient’s health complexity. Without specificity, a patient’s chronic conditions may be underrepresented, potentially impacting both care planning and practice revenue.
CMS guidance stresses coding to the highest level of specificity to ensure proper reimbursement. Similarly, the CDC’s ICD-10-CM guidelines highlight that accurate codes give a clearer picture of a patient’s health status.
The Risk Adjustment Connection
Risk adjustment is more than a billing tool—it’s a measure of patient complexity.
- In CMS-HCC models, each chronic condition contributes to a patient’s risk score.
- Underdocumenting or using unspecified codes can understate a patient’s health burden, leading to lower payments for practices managing higher-risk populations.
- Accurate, specific diagnoses ensure that patients’ risk profiles are captured, enabling appropriate care management and financial sustainability.
AAPC and AHIMA emphasize that capturing all relevant conditions, including comorbidities, maximizes both care quality and reimbursement.
How BCA Helps Practices Optimize Specificity and Risk Capture
At BCA, we support healthcare organizations in achieving accurate documentation, coding, and risk-adjusted reimbursement.
- Chart Audits and Risk Adjustment Reviews
BCA performs detailed audits across specialties—including medical, behavioral health, FQHCs, RHCs, and dental—to identify where diagnoses are vague or under-coded. These audits highlight opportunities to improve both specificity and HCC capture.
- Provider Education
We offer group and one-on-one training for clinicians and staff, focusing on:
- Proper documentation of chronic conditions
- Coding to the highest level of specificity
- Capturing all relevant risk-adjusted diagnoses
These programs ensure that your team is equipped to support both patient care and accurate reimbursement.
- Fractional Revenue Cycle Support
For practices facing staffing or budget constraints, BCA offers flexible fractional revenue cycle services, helping maintain coding accuracy, compliance, and risk adjustment capture without hiring full-time staff.
Bottom Line
Specificity in diagnosis coding is no longer optional—it’s a cornerstone of:
- High-quality patient care
- Accurate, timely reimbursement
- Effective risk adjustment capture
By partnering with an experienced organization like BCA, healthcare providers can navigate the complexities of coding, improve documentation, optimize revenue, and ensure that patients’ conditions are fully recognized and managed.
Missed codes = missed revenue. Don’t leave dollars on the table.
Book your consultation today with one of our experts.