Every missed chronic condition revalidation can mean lost revenue, missed care opportunities, and extra headaches for your team. For primary care providers in FQHCs navigating tighter Medicaid budgets, increasing reporting requirements, and packed schedules, keeping up with revalidation can feel impossible. Yet missing it doesn’t just affect your bottom line—it can compromise patient care and program eligibility.
Today, we’ll talk about how to embed chronic condition revalidation into your daily workflow—making it automatic, streamlined, and part of the routine without adding time to your day.
Identify Where Revalidation Slips
Most missed revalidations happen at three points: pre-visit planning, during the visit, and post-visit. Maybe the problem list isn’t updated, key conditions aren’t fully addressed in notes, or follow-up flags are ignored. Ask yourself: “Where in my day does revalidation fall through?” Pinpointing these gaps is the first step toward fixing them.
Use EHR Prompts Smartly
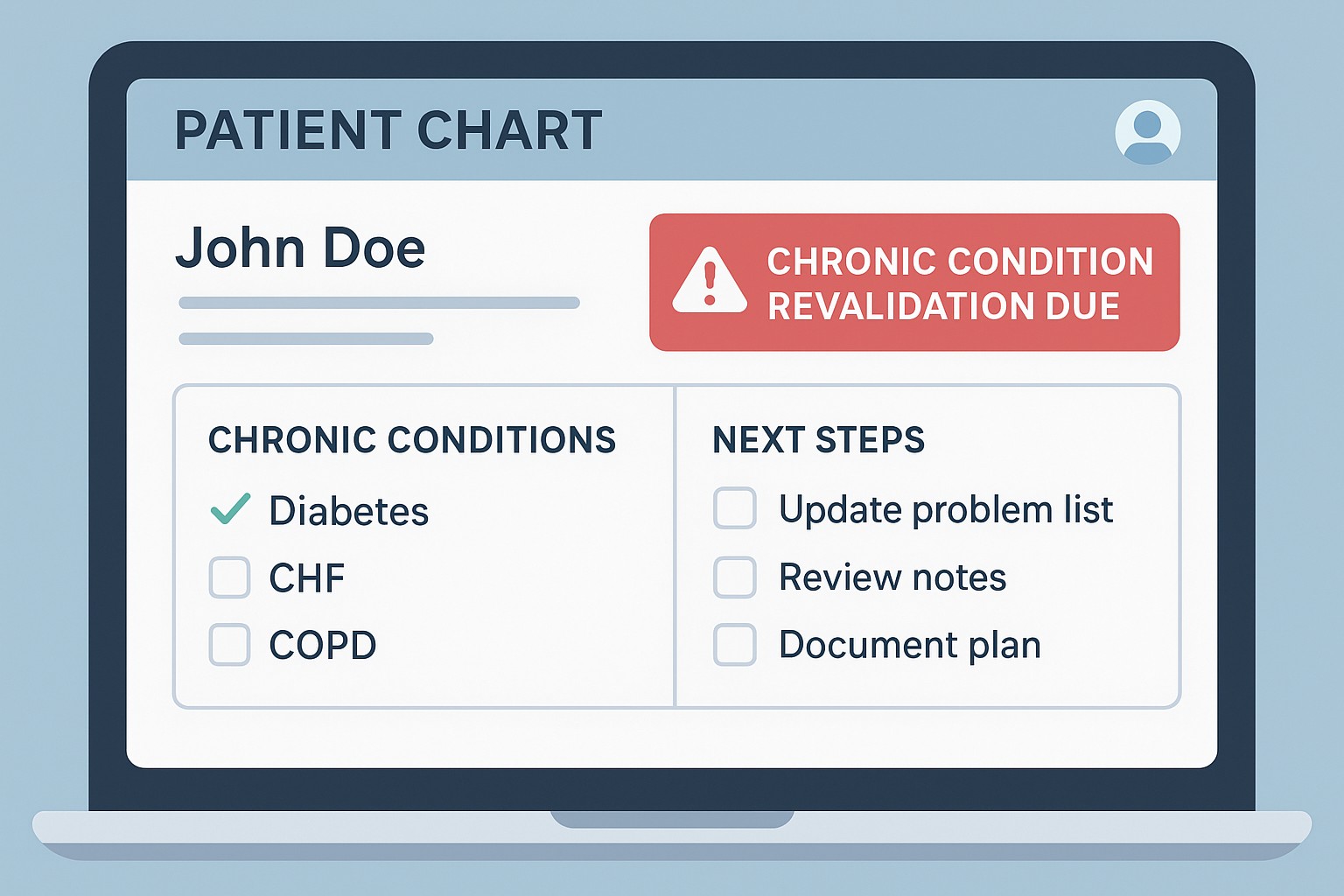
Dashboards or health maintenance reminders can flag “Revalidation Due” for chronic conditions like CHF, diabetes, or COPD. Configure them to appear before or at the start of the visit and fire annually unless an assessment and plan are documented.
Smart templates go further. AWVs, CCM visits, or chronic-condition visits can include structured problem list reviews, drop-downs for status, and auto-fill fields for labs or vitals. Prompts like “Review and confirm each chronic condition listed” help providers avoid relying on memory alone.
Make It a Team Effort
Medical assistants and nurses can run pre-visit checklists noting conditions not addressed in the past 12 months, last documentation dates, and active revalidation flags. Even adding a simple column in the schedule view showing “Active Chronic Conditions Not Addressed in 12M” can make a big difference.
During the visit, templates or smart phrases (e.g., .revalcheck) prompt providers to confirm active conditions, link labs and medications, and track care gaps. Post-visit, coders and quality teams can generate reports highlighting patients missing annual documentation or notes without linked diagnoses.
Keep Alerts Lean
Avoid alert fatigue by prioritizing high-value conditions and limiting prompts to annual follow-ups. Tiered prompts—showing only overdue conditions unless clicked—keep workflows clean.
Key Takeaway: Revalidation isn’t extra work—it’s embedding checks into what you already do. With pre-visit prep, smart templates, light prompts, and a team-based approach, chronic condition revalidation becomes seamless. Everyone shares responsibility, providers focus on care, and documentation and coding reflect the work being done.
Next Steps: If your clinic is ready to put these strategies into action, BCA’s team can help. Through targeted audits, personalized education, and hands-on consulting, we ensure that your workflows not only support accurate chronic condition documentation but also strengthen coding, risk adjustment, and program eligibility.
Book your consultation with BCA today to make revalidation a routine part of every patient encounter.